Some of the professional groups that have published findings in support of cranial remolding programs for this patient population include:
- American Academy of Orthotists & Prosthetists (AAOP)
- American Academy of Pediatrics (AAP)
- American Association of Neurological Surgeons (AANS)
- American Nurses Association (ANA)
- American Physical Therapy Association (APTA)
- American Society of Maxillofacial Surgeons (ASMS)
- Congress of Neurological Surgeons (CNS)
- National Institute of Child Health and Human Development (NICHD)
- National Institute of Health (NIH)
Deformational plagiocephaly and other head shapes are estimated to be present in up to 20% of all infants.
The weight of the clinical evidence and a preponderance of clinical data supports cranial remolding programs for infants with moderate to severe deformities. The success of these orthotic treatment programs depends on the age of the infant, severity of deformity, compliance with the wearing schedule, clinical expertise of the cranial orthotist, and quality of the cranial design. This is supported by many multidisciplinary publications associated with evidence-based practices, systematic reviews, position statements, clinical practice guidelines and best practices.
Restricted Growth
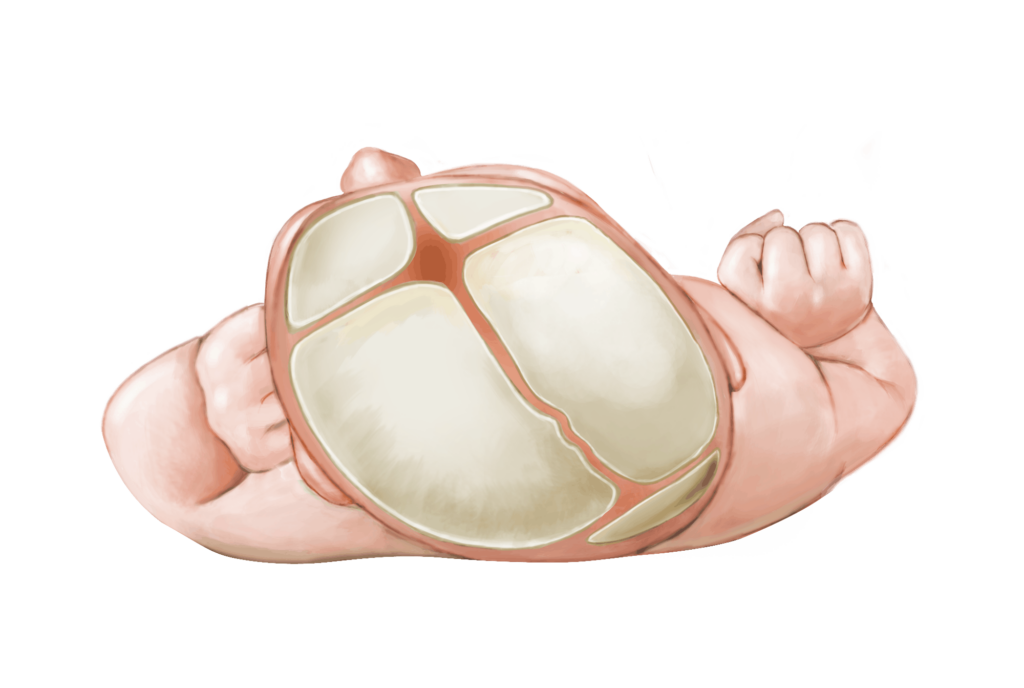
Many factors contribute to the development of abnormal head shapes in infants. These may include but are not limited to: in-utero restrictions, primigravida, neck muscle imbalances or torticollis, preferred postures, sustained supine positioning, concurrent medical conditions, prematurity, hypotonia, etc.
Repositioning efforts are most effective in the first 3 – 4 months after birth, and may have a significant impact on overall head symmetry and proportion.

Sustained supine positioning

Torticollis
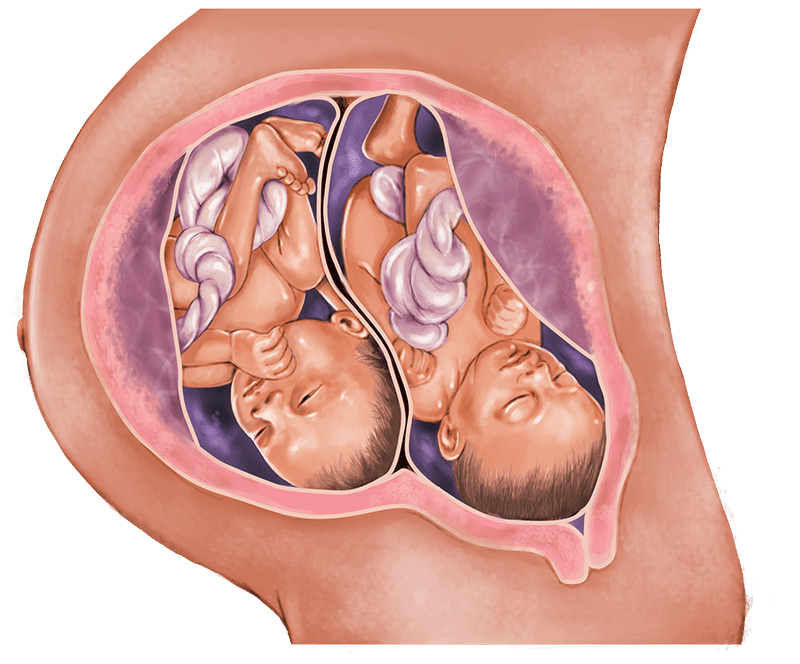
In-utero restrictions
Unrestricted Growth
Babies become more active by six months of age, and most are sitting up and exploring their surroundings. Decreasing the duration of restrictive forces by rolling and sitting likely decreases the continued deformation. Now the brain continues to grow along the path of least resistance in all dimensions and directions, however, there is no internal mapping program that restricts growth in certain regions and promotes growth in others. The brain simply grows and pushes on the skull in a constant and consistent manner. As such, the head shape stays the same while the head size increases. In some cases, this increase in size makes the deformity seem less apparent, but directed growth will not occur without the correct placement of resistive forces over bossed areas.
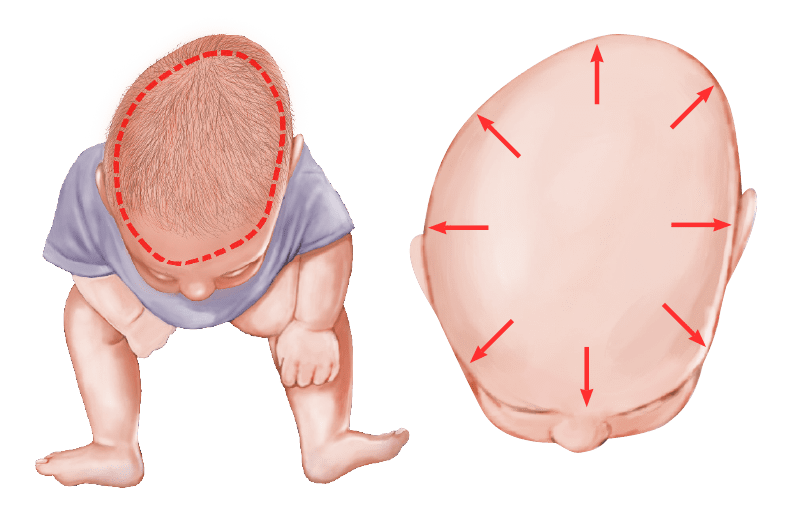
Head growth follows path of least resistance
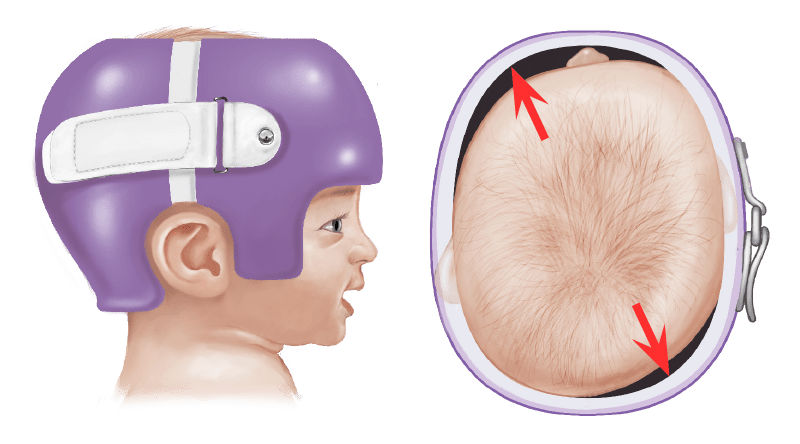
Directed Growth
Mild asymmetries and disproportions are common and should not cause concern. If a moderate or severe head deformity remains after a period of focused repositioning, orthotic evaluation and considerations are warranted. A cranial remolding orthosis provides appropriate resistance over the bossed areas so that natural brain and skull growth is directed into the areas of flattening. Earlier orthotic treatment for younger infants produces optimal results in the shortest period of time.
Advancements in Clinical Care
The references listed below represent the findings of interdisciplinary groups relative to the support of cranial remolding orthoses for the treatment of deformational plagiocephaly. This list is intended to provide a summary of key findings and is in no way intended to cover the entire scientific body of knowledge about deformational plagiocephaly, repositioning, therapy and orthotic treatment. Important findings are listed for each publication as they relate to appropriate diagnosis, prescription criteria, referral pathways and outcomes for infants identified with skull deformities.
Clinical Classification of Positional Plagiocephaly
Journal of Craniofacial Surgery (2004)
IMPORTANT FINDINGS: Classification technique is highly reproducible, cost effective and easy to understand • Identified 5 types of deformational plagiocephaly and 3 types of deformational brachycephaly with increasing components of deviation and severity • Infants older than 4 months with Type II or higher, or infants non-responsive to repositioning are recommended for orthotic care • The younger the infant at the initiation of the helmet program, the faster the resolution of the head deformity
Louis Argenta, MD
Comparison of Infant Head Shape Changes in Deformational Plagiocephaly Following Treatment with a Cranial Remolding Orthosis Using a Noninvasive Laser Shape Digitizer
Journal of Craniofacial Surgery (2006)
IMPORTANT FINDINGS: Identified four anthropometric measurements significant to correction of deformational plagiocephaly • Developed the CHOA Plagiocephaly Severity Scale that includes clinical characteristics for diagnosis, quantitative measures for severity and clinical recommendations for treatment • Treatment with cranial remolding orthoses (CROs) significantly alters head shape and improves symmetry
Laura Plank CO; Brian Giavedoni, CP; Janet Lombardo, CPO; Mark Geil, PhD; Andrew Reisner, MD
CLINICAL REPORT: Prevention and Management of Positional Skull Deformities in Infants
Pediatrics (2011)
IMPORTANT FINDINGS: The pediatrician is the gatekeeper for the diagnosis and successful management of pediatric deformational skull conditions • Pediatricians should examine and educate parents about deformational plagiocephaly in the newborn period, and monitor for improvement or progression • Repositioning is recommended for mild to moderate deformities • Repositioning and molding helmets are options for infants with moderate to severe deformities • Cranial orthoses are especially effective for severe deformities and for infant head shapes non-responsive to repositioning efforts • Pediatricians should manage referrals to physical therapists and cranial orthotists • Referrals to craniofacial specialists should be considered for complex presentations or suspicion of craniosynostosis
James Laughlin; Thomas G. Luerssen; Mark S. Dias; Committee on Practice and Ambulatory Medicine, Section on Neurological Surgery; American Academy of Pediatrics
Evidence-Based Care of the Child with Deformational Plagiocephaly, Part I: Assessment and Diagnosis
Journal of Pediatric Health Care (2012)
IMPORTANT FINDINGS: Systematic review/grading from 2000-2011• Develop-mental assessment is an essential part of patient management • Important to identify and manage torticollis • Pediatric primary care providers are competent to diagnose deformational plagiocephaly • Significance of anthropometric measurements compared to age-related norms or individual’s previous measurements (e.g. cephalic index and transcranial diagonal difference or cranial vault asymmetry) • Anthropometric measurements defined three levels of severity for both deformational plagiocephaly and brachycephaly based upon a synthesis of the published literature
Wendy Looman, PhD, RN, CNP; Amanda Kack Flannery, RN, CNP
Evidence-Based Care of the Child with Deformational Plagiocephaly, Part II: Management
Journal of Pediatric Health Care (2012)
IMPORTANT FINDINGS: Systematic review/grading from 2000–2011 • Developed evidence-based clinical decision tool • Repositioning is the most conservative treatment up to 4 months of age • CROs for infants 6 months or older, or for infants with severe asymmetry regardless of age • Decisions regarding treatment with CROs best made by 6 months of age
Amanda Kack Flannery, RN, CNP; Wendy Looman, PhD, RN, CNP; Kristin Kemper, RN, CNP
Cranial Molding Helmet Therapy and Establishment of Practical Criteria for Management in Asian Infant Positional Head Deformity
Child’s Nervous System (2014)
IMPORTANT FINDINGS: Over 1000 infants underwent molding helmet therapy after being diagnosed with deformational plagiocephaly • Evaluation of anterior, posterior and overall skull symmetry • Improved outcomes were found in the severe group when treatment was initiated earlier • Treatment was especially effective when initiated at 4 months of age • Better outcomes were obtained with earlier treatments • Molding helmet therapy is effective with early identification and appropriate timing of the treatment program • The misconception that an infant’s head “will round out on its own as the child becomes more active, begins to roll over and learns to sit up” is based on outdated scales of motor development and a lack of appreciation for the effect of sustained supine positioning • Pediatricians must be aware of the time-sensitive nature of cranial remolding programs to optimize outcomes
Yasuo Aihara, Kana Komatsu, Hitoshi Dairoku, Osami Kubo, Tomokatsu Hori, Yoshikazu Okada
Effectiveness of Conservative Therapy and Helmet Therapy for Positional Cranial Deformation
Plastic and Reconstructive Surgery (2015)
IMPORTANT FINDINGS: More than 4000 patients identified and treated with repositioning, repositioning and therapy, or cranial remolding orthosis • Deformational plagiocephaly can be managed with conservative therapy and cranial remolding orthoses and are guided by patient-specific risk factors • CROs address external factors that limit the effectiveness of repositioning efforts • CROs may be the preferable course of treatment at the outset • Delaying the initiation of helmet therapy for a trial course of repositioning does not prevent correction of the deformity as long as the orthotic treatment is begun during the appropriate period of growth and families are compliant with the wearing schedule • In the cranial remolding orthoses treatment group, complete correction was achieved in 95.0 percent of patients
Jordan P. Steinberg, MD, PhD, Roshni Rawlani, BA, Laura S. Humphries, MD, Vinay Rawlani, MD, Frank A. Vicari, MD
Summary: Evidence Based Guidelines for the Treatment of Pediatric Positional Plagiocephaly
Congress of Neurological Surgeons (2016)
IMPORTANT FINDINGS: Guidelines endorsed by the American Academy of Pediatrics • Diagnosis of deformational plagiocephaly is made by physical examination • Repositioning is most effective for infants 4 months or younger • Helmets are especially effective for severe deformities • Physical therapy is more effective than repositioning for severe cases • Cranial remolding orthoses are indicated for infants over 8 months of age with significant deformities or younger infants non-responsive to repositioning or physical therapy • Helmets are more effective than therapy for severe asymmetry and must be provided during the appropriate period of growth during infancy • Infants with severe deformities who are treated early will obtain better outcomes
Ann Marie Flannery, MD; Mandeep S. Tamber, MD, PhD; Catherine Mazzola, MD; Paul Klimo Jr., MD; Lissa C. Baird, MD; Rachana Tyagi MD; David Bauer, MD; Alexandra Beier, DO; Susan Durham, MD; Alexander Y. Lin, MD; Catherine McClung Smith, MD; Laura Mitchell; Dimitrios Nikas, MD
Congress of Neurological Surgeons Systematic Review and Evidence-Based Guideline on the Role of Cranial Molding Orthosis (Helmet) Therapy for Patients with Positional Plagiocephaly
Neurosurgery (2016)
IMPORTANT FINDINGS: There is a preponderance of nonrandomized evidence to support more significant and faster improvements in infants with deformational plagiocephaly when treated with CROs compared to more conservative measures • CROs are especially indicated for severe deformities • CROs must be provided during the appropriate period of growth during infancy • Infants with more severe deformities and infants who are helmeted at earlier ages have more significant outcomes and even normalization of head shape
Mandeep S. Tamber, MD, PhD; Dimitrios Nikas, MD; Alexandra Beier, DO; Lissa C. Baird, MD; David Bauer, MD; Susan Durham, MD; Paul Klimo Jr., MD; Alexander Y. Lin, MD; Catherine Mazzola, MD; Catherine McClung Smith, MD; Laura Mitchell; Rachana Tyagi MD; Ann Marie Flannery, MD
Plagiocephaly Severity Scale to Aid in Clinical Treatment Recommendations
Journal of Craniofacial Surgery (2017)
IMPORTANT FINDINGS: Provides additional validation for the CHOA Plagiocephaly Severity Scale used to classify clinical presentation and severity of skull deformities • CHOA scale assists in the development of a clinical treatment plan • Provides a low-cost solution for measuring severity in a clinical setting • Details observational characteristic and qualitative differences related to varying degrees of severity • CHOA scale is an efficient and reproducible method to evaluate qualitative and quantitative components of the clinical presentation and create an effective treatment recommendation and program
Mark A. Holowka, MSPO, CPO Andrew Reisner, MD; Brian Giavedoni, MBA, CP; Janet R. Lombardo, MBA; CPO Colleen Coulter, DPT, PhD
Plagiocephaly and Developmental Delay: A Systematic Review
Journal of Developmental and Behavioral Pediatrics (2017)
IMPORTANT FINDINGS: Infants identified with misshapen skull often present with developmental delays, primarily motor followed by language • Plagiocephaly is identified as a marker for a higher risk of developmental concerns and clinicians should screen and monitor these infants • Early intervention with physical therapy may help to decrease the effects of motor delays and also identify infants in need of longer term developmental programs • Developmental assessments are warranted for all infants identified with plagiocephaly • Pediatricians / clinicians should screen for skull deformities and motor delays and promote early referrals for appropriate therapeutic interventions
Alexandra Martiniuk, Cassandra Vujovich-Dunn, Miles Park, William Yu, Barbara Lucas
Deformational Plagiocephaly: A Review
Pediatric Nursing (2017)
IMPORTANT FINDINGS: Deformational plagiocephaly is a common condition in infancy • Characterized by asymmetrical distortion of the skull • Nurses have a key role in the identification and prevention, and education of parents • Risk factors include sociodemographic, obstetric/perinatal, infant characteristics and infant care practices • CROs recommended for infants with moderate to severe deformational plagiocephaly, signs of facial deformities, signs of developmental delay, and whose head shape does not improve with repositioning • Prevention includes educating parents about repositioning strategies and tummy time activities while infants are still very young
Kanlaya Ditthakasem, John Kolar
Facial Asymmetry Correction with Moulded Helmet Therapy in Infants with Deformational Skull Base Plagiocephaly
Journal of Cranio-Maxillo-Facial Surgery (2018)
IMPORTANT FINDINGS: Severe presentations of deformational plagiocephaly is often accompanied by facial asymmetry, ear shift, and disruptions to the skull base • Cranial remolding orthoses have become an accepted treatment regimen for infants with skull deformities • Moulding helmet therapy reduced ear shift, improved TMJ position, and improved facial asymmetry within 5 months of treatment • Cranial remolding orthoses can correct facial asymmetry and associated basal skull asymmetry in infants with deformational plagiocephaly
Matthias Kreutz, Brigitte Fitze, Christoph Blecher, Augello Marcello, Ruben Simon, Rebecca Cremer, Hans-Florian Zeilhofer, Christoph Kunz, Johannes Mayr
Prevalence and Characteristics of Positional Plagiocephaly in Healthy Full-Term Infants at 8-12 Weeks of Life
European Journal of Pediatrics (2018)
IMPORTANT FINDINGS: Deformational plagiocephaly is a common issue • Argenta’s assessment tool used to examine 283 healthy infants • 107 (37.8%) had deformational plagiocephaly at 8–12 weeks of age • 64.5% had right occipital flattening • 50.5% were male • 15% also presented with deformational brachycephaly • Need to provide uniform messages prenatally and postnatally (prevention and repositioning)
E Ballardini, M Sisti, N Basaglia, M Benedetto, A Baldan, C Borgna-Pignatti, G Garani
The Role of Age on Helmet Therapy in Deformational Plagiocephaly and Asymmetric Brachycephaly
Child’s Nervous System (2019)
IMPORTANT FINDINGS: Retrospective review of 98 infants with deformational plagiocephaly and asymmetrical brachycephaly • Patients with deformational plagiocephaly identified by a cranial vault asymmetry index (CVAI) ≥7% and a cranial vault asymmetry (CVA) ≥10mm • Patients with deformational asymmetrical brachycephaly identified by a cranial vault asymmetry index (CVAI) ≥7% and a cephalic ratio (CR) ≥94% • Group 1 initiated orthotic treatment prior to 6 months of age, Group 2 initiated orthotic treatment after 6 months of age • Findings support efficacy of cranial remolding orthoses for infant skull deformities • Helmet therapy should be initiated before 6 months of age for optimal outcomes
S Cevik, S Isik, A Ozkilic
A New Parameter for the Management of Positional Plagiocephaly: The Size of the Anterior Fontanelle Matters
Child’s Nervous System (2019)
IMPORTANT FINDINGS: Goal to compare the results of physical therapy and helmet treatment, and to investigate the influence of the size of the anterior fontanelle • Skull remolding rate was significantly higher with cranial remolding orthosis treatment than with physical therapy • Patients with a small fontanelle had a lower spontaneous remolding rate • Skull correction occurred significantly faster with CRO treatment, especially for infants with smaller fontanelles • Patients with smaller fontanelles may benefit from earlier helmet therapy than their counterparts with larger fontanelles
DS Wendling-Keim, Y Mace, H Lochbihler, HG Dietz, M Lehner
Effects of Initial Age and Severity on Cranial Remolding Orthotic Treatment for Infants with Deformational Plagiocephaly
Journal of Clinical Medicine (2019)
IMPORTANT FINDINGS: Retrospective chart review of 499 infants with non-synostotic plagiocephaly who completed CRO treatment • Subgroups identified by age at initiation of treatment and severity of skull deformity • Treatment times increased with initial severity and infant age • Younger infants with less severe skull deformities have shorter treatment times and less residual cranial deformation after CRO treatment • Older infants had longer treatment times and less correction of skull deformities • Clinical considerations must include the age of the infant and initiating CRO treatment prior to progression of the cranial deformity
Tiffany Graham, Beverley Adams-Huet, Nicole Gilbert, Kirsten Witthoff, Terran Gregory, Mary Walsh
Significant Factors Influencing the Effectiveness of Cranial Remolding Orthoses in Infants with Deformational Plagiocephaly
Journal of Craniofacial Surgery (2019)
IMPORTANT FINDINGS: Torticollis and prematurity are risk factors for cranial deformities • Younger infants have faster and greater skull correction with cranial remolding orthoses • Presenting age, presenting severity and the presence of torticollis are factors that significantly influence the duration of treatment with CROs • Presenting age and severity also significantly influence final head shape
Tiffany Graham, Nicole Gilbert, Kirsten Witthoff, Terran Gregory, Mary Walsh